Last year alone, the U.S. healthcare sector suffered an unprecedented 276 million breached records, driven by a ransomware attack that compromised data for 190 million people.
The HIPAA Journal reports that healthcare organizations face nearly two major data breaches daily, with cybercriminals relentlessly targeting valuable patient information. But the risks extend far beyond cyberattacks.
Hospitals must also contend with physical threats as workplace violence now accounts for 73% of all nonfatal injuries in healthcare, and theft of medical equipment costs the industry billions annually. These realities make regular, comprehensive security assessments essential for protecting patients, staff, and your organization’s reputation.
In this 2025 Hospital Security Assessment guide, let's explore how to identify vulnerabilities, address emerging threats, and ensure compliance with evolving standards.
What is a Hospital Security Assessment?
A hospital security assessment is a comprehensive evaluation of a healthcare facility’s physical and digital security infrastructure. It involves a systematic review conducted by trained security professionals, often in collaboration with hospital administrators, to identify potential vulnerabilities and areas for improvement.
The process includes:
- Reviewing building layout and access points (entrances, exits, restricted zones, emergency routes)
- Assessing surveillance systems and coverage
- Evaluating alarm and emergency response systems
- Inspecting access control measures
- Analyzing cybersecurity protocols
- Identifying potential physical and digital threats
- Recommending improvements for overall safety
The goal is to determine how effectively the hospital can prevent, detect, and respond to threats such as unauthorized access, data breaches, theft, or violence. Based on the findings, security professionals provide recommendations to enhance protection for patients, staff, data, and assets, providing a safer, more resilient healthcare environment.
The Importance of Security in Hospitals
Doctors, nurses, and healthcare teams need to feel safe where they work to give their best. A secure hospital environment protects patients from risks like physical violence, medication misuse, and data breaches while focusing on care.
At the same time, hospitals must meet strict regulations related to patient safety, controlled substances, and private health information. Sensitive areas like pharmacies require extra attention to prevent theft or misuse of medications. Falling short in these areas risks patient well-being and can lead to heavy fines or even legal action.
- Workplace Safety
Healthcare professionals need to feel secure to provide the highest quality of care. Unfortunately, hospitals are increasingly sites of workplace violence as healthcare staff are five times more likely to experience violence than workers in other sectors, and aggravated assaults account for 78% of violent crimes in these settings.
A staggering 72% of healthcare workers report concerns about rising patient violence. Security assessments help identify vulnerable areas, improve incident response, and foster a safer environment for staff and patients alike.
- Protection of Assets and Medications
Hospitals are home to valuable assets and controlled substances. The theft and misuse of medications cost facilities up to $164 million annually, while medical equipment theft adds another $4 billion in losses.
Security assessments help pinpoint weak spots in physical security, such as unsecured pharmacies or easily accessible equipment storage, enabling targeted improvements to prevent costly losses.
- Safeguarding Patient Data
With healthcare data breaches impacting 116 million Americans in 2023 and the average breach costing $10.93 million, protecting patient information has never been more paramount. Physical security lapses can lead to unauthorized data access, resulting in HIPAA violations and severe financial penalties. Regular assessments ensure that access controls, surveillance, and data protection measures are up-to-date and effective.
- Regulatory Compliance
Hospitals must comply with stringent regulations governing patient safety, medication handling, and data privacy. Security assessments help institutions stay ahead of compliance requirements, reducing the risk of legal action, fines, or reputational damage.
Risk Assessment vs Risk Management
In healthcare, keeping patients and staff safe is more than a priority. Every day, hospitals face a wide range of risks that can affect patient care, staff wellbeing, and the overall functioning of the facility. From physical hazards like slippery floors to cybersecurity threats that could expose sensitive patient data, understanding these risks is the first step toward handling them effectively.
But how do hospitals actually handle safety risks? Through hospital security risk assessment and risk management.
Risk assessment is a careful look at what might go wrong, identifying and analyzing such hazards.
- For example, hospital leaders and staff might review emergency exits to check if they’re clear and functional, or assess if medication storage areas are secure enough to prevent theft or errors.
- This process involves listing possible dangers, figuring out how likely they are to happen, and understanding what the consequences could be. Think of it as mapping out all the potential “what ifs” before they happen.
But knowing about risks alone doesn’t keep a hospital safe. That’s where risk management steps in.
- Once risks are identified, risk management is the ongoing process of deciding what to do about them. This means developing and putting into practice solutions to reduce or eliminate risks.
- For example, if a hospital security risk assessment finds that emergency exits are blocked during busy shifts or staff aren’t always checking patient ID bands properly, risk management might include updating staff training, regular audits, changing cleaning schedules, or installing alarms to alert if exits are obstructed.
Risk management also includes monitoring how well these solutions work over time. It’s a continuous cycle of reviewing risks, acting on them, and adjusting as needed.
Everyone in the hospital from administrators to frontline staff needs to work together for risk management to be effective. Without this continuous effort, risks go unmanaged, and the safety of everyone in the hospital is at stake.
To sum it up in simple terms:
- Risk assessment asks: What can go wrong?
- Risk management answers: What are we doing about it?
Both parts are essential and must work hand in hand to create a safe healthcare environment. By understanding and applying both risk assessment and risk management, healthcare facilities create safer spaces where staff can focus on care without worry, and patients can feel secure and protected.
Key Components of a Hospital Security Assessment
Every corner of a hospital holds critical risks, from physical safety to data privacy. To conduct a successful hospital security assessment, stakeholders must thoroughly evaluate existing security measures and how effectively they protect patients, staff, and the facility from physical and digital threats. A well-rounded hospital security system typically encompasses several key elements.
Each of the following components in hospital security risk assessment plays a vital role in assessing the strength of the overall security strategy and identifying any vulnerabilities or areas that require improvement:
1. Physical Security Evaluation
Hospitals are open environments as people (patients, families, emergency responders) come in and out at all hours. This openness, while essential, creates unique vulnerabilities. A physical security review checks whether the current safeguards are doing their job.
- Entrances and exits: Are they appropriately monitored? Are access controls in place in restricted areas like ICUs or pharmacy stores?
- Access Control Systems: Assess the use of electronic locks, key cards, and biometric systems. Are restricted areas properly protected? Are visitor management processes clearly defined?
- Video Surveillance: Evaluate camera placement, coverage, clarity, and integration with centralized monitoring systems. Coverage should include emergency departments, entrances, hallways, and parking lots. Blind spots must be eliminated.
- Alarm Systems and Sensors: Ensure alarms are functional, cover key zones, and are configured to trigger immediate responses.
- Perimeter Security: Inspect fences, gates, bollards, and entry/exit points like ER entrances and parking lots.
- Emergency Response Readiness: Review evacuation maps, lockdown capabilities, and the presence of trained onsite security personnel.
2. Risk Assessment & Threat Identification
Understanding potential threats is essential to developing a targeted security plan. Risk assessment identifies vulnerabilities unique to the hospital's location, operations, and previous history.
- Past Incident Review: What types of incidents have occurred before? Theft, trespassing, aggressive behavior, or cyberattacks?
- Crime Trends: Consider local crime data to understand external risks like theft, vandalism, or violence. A facility in a high-risk area might need added physical and personnel security.
- Environmental Factors: Assess potential natural disaster risks, such as floods, earthquakes, or extreme weather.
- Threat Scenarios: Simulate realistic threat scenarios (e.g., active shooter, data breach, utility failure) to assess the impact and identify mitigation steps.
3. Regulatory Compliance
Security assessments must ensure the facility aligns with federal, state, and industry regulations. Non-compliance can lead to legal consequences, financial penalties, and loss of trust.
- HIPAA: Patient data protection standards for both physical and electronic information.
- OSHA: Workplace safety standards for both clinical and non-clinical staff.
- CMS Emergency Preparedness Requirements: Ensures hospitals are ready to handle disasters, pandemics, and violent threats.
- DEA Regulations: Secure handling and tracking of controlled substances.
- Building Codes & Fire Safety Laws: Basic infrastructure compliance is non-negotiable.
4. Vulnerability Testing
This is where the security team moves from planning to testing. Vulnerability assessments simulate attacks to test how easy it is to bypass current defenses. These tests provide valuable insights into how systems and personnel would fare under pressure.
- Penetration Testing: Simulated hacking attempts on digital systems to find weak points in the network, software, or devices.
- Physical Pen Tests: Trying to access restricted areas without permission to see if unauthorized access is possible.
- Social Engineering Tests: Test how staff react to phishing attempts, tailgating, or phone scams. These exercises reveal human factors that technology alone can't fix.
5. Emergency Preparedness Evaluation
Hospitals must be ready for various emergencies, from fire alarms and natural disasters to violent intruders and large-scale disease outbreaks. A security assessment should include a comprehensive review of emergency plans and readiness. A plan that exists only on paper is no help in a real emergency. Real-world testing is what saves lives.
- Crisis Management Plans: Evaluate the hospital’s documented plans for incidents like active shooters, fires, or natural disasters.
- Lockdown & Evacuation Procedures: Staff must know where to go and what to do during a crisis.
- Staff Training: Confirm that all staff are trained on response protocols, including communication chains and roles during emergencies.
- Drills & Simulations: Regularly test emergency plans with realistic simulations to identify procedural or training gaps.
6. Cybersecurity Review
Hospitals hold enormous volumes of sensitive data, including electronic health records, billing information, lab results, and more. A hospital security assessment must include a thorough cybersecurity evaluation.
- Firewalls & Encryption: Are data transfers and storage encrypted? Are firewalls configured to block unauthorized access?
- Endpoint Protection: Are all connected devices protected from malware and breaches?
- Access Management: Who can access what, and are permissions regularly reviewed?
- Patch Management: Are software and systems up to date with security patches?
- Backup and Recovery: Is the hospital prepared for a ransomware attack or data loss?
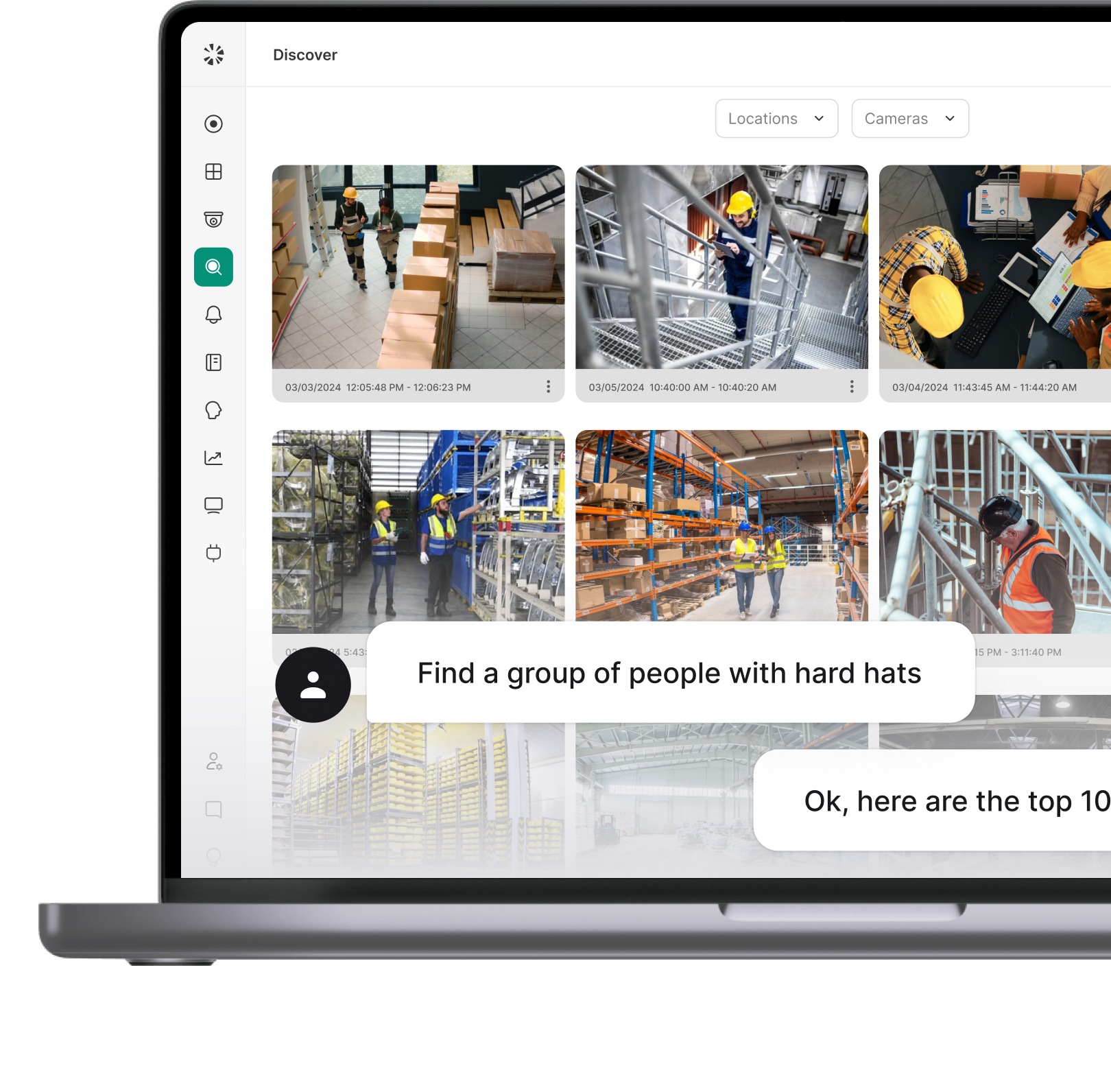
7. Technology Integration
Having security tools is not enough—they need to work in sync. This part of the assessment looks at how well the hospital’s systems are integrated and managed. Smooth integration avoids delays, miscommunication, and errors during emergencies.
- Unified Security Platforms: Combine video surveillance, access control, alarm systems, and IoT monitoring into one control center.
- AI & Analytics: Use machine learning to detect anomalies, such as unauthorized access attempts or movement in restricted areas.
- Environmental Sensors: Monitor factors like air quality, humidity, and temperature—especially crucial in sensitive zones like operating rooms or pharmaceutical storage.
8. Policy and Procedure Review
Policies guide everyday actions. Even the best technology can be undermined by poor policies or inconsistent enforcement. If they are outdated or unclear, staff may not know how to act when a security issue occurs. A security assessment must include a deep dive into written policies and real-world practices.
- Access Policies: Who is allowed, where, and how is that controlled? How are access credentials issued, updated, and revoked?
- Controlled Substance Management: Are drugs stored, tracked, and disposed of securely?
- Incident Reporting: Are there clear, standardized processes for reporting and documenting security incidents?
- Data Protection: Are there privacy policies aligned with national and local regulations?
- Response Protocols: Are procedures for bomb threats, missing patients, or hostile visitors clear and practical?
9. Staff Awareness and Training
The best security systems may fail if staff don’t know how to use them or recognize threats. Human behavior is often the weakest link in security. A strong assessment includes evaluating how well employees understand their role in maintaining security.
- Emergency response drills (e.g., fire, lockdown)
- Reporting procedures for suspicious activity
- Recognizing phishing attempts and social engineering
- De-escalation tactics in patient and visitor interactions
Why Are Security Risk Assessments Important?
- Identify Security Gaps
Risk assessments help uncover weaknesses in physical, digital, and procedural systems. Whether it's a door without proper access control, outdated software, or a lapse in emergency protocols, identifying these gaps allows hospitals to take corrective action before they become serious threats.
- Reduce Long Term Costs
Preventing security incidents is far less expensive than dealing with their aftermath. Risk assessments help avoid costly breaches, fines, operational downtime, and potential lawsuits, saving the organization from major financial setbacks in the long run.
- Mitigate & Protect Against Breaches
A thorough assessment highlights vulnerabilities that could lead to data breaches or unauthorized access. By addressing these risks early, hospitals can strengthen their defenses and protect sensitive patient information, medical equipment, and staff safety.
- Help Budget Future Security Initiatives
Assessments provide clarity on where security investments are needed most. This makes it easier for decision-makers to plan and allocate budgets for technology upgrades, training programs, or infrastructure improvements based on actual risks, not assumptions.
- Increases Employee Security Awareness
When staff are involved in or informed about security assessments, it boosts their awareness and accountability. Employees become more cautious, better at spotting unusual activity, and more likely to follow protocols, creating a stronger, security-conscious culture throughout the facility.
How to Prepare for a Hospital Security Assessment
Step 1 - Define Assessment Objectives
Begin by clearly outlining what the hospital hopes to achieve through the security assessment. This includes identifying the areas of highest concern—such as physical security, cybersecurity, emergency preparedness, or employee safety.
- Look at past incidents like break-ins, data breaches, or internal thefts to pinpoint patterns or vulnerabilities.
- Reviewing local crime data also helps understand external risks.
For example, if the hospital has experienced multiple physical intrusions or confrontations in the ER, then improving access control and staff safety should be top priorities. Setting clear objectives early on allows teams to stay focused and make the assessment relevant to the hospital’s unique challenges. It also makes sure the results lead to actionable steps and measurable improvements in security.
Step 2 - Identify Threats and Vulnerabilities
The next critical step is identifying all potential threats that could impact the safety and operations of the hospital. This includes both man-made risks, such as theft, violence, or vandalism, and natural hazards like fires, floods, or power outages.
Security teams must assess which areas, systems, or assets are most vulnerable; such as emergency rooms, data servers, or controlled drug storage. It's also important to assign risk ratings to each threat based on likelihood and impact. These ratings are typically based on past incidents, the hospital’s physical layout, and local crime trends.
By identifying and prioritizing vulnerabilities, the assessment process becomes more focused and practical. Teams can direct attention and resources to areas that carry the highest risk.
Common threats include:
- Acts of aggression or verbal abuse
- Active shooter situations
- Theft or vandalism
- Arson or sabotage
- Terrorism threats
- Data breaches and cyberattacks
Step 3 - Propose Risk Mitigation Measures
Once threats and vulnerabilities have been identified, the next step is to propose effective and realistic risk mitigation strategies. The assessment team must analyze findings, weigh the likelihood of each threat, and compare it to the potential impact. This allows for prioritization ensuring that limited budgets are directed toward the most critical areas.
Stakeholders should also assess the institution’s financial capacity to support necessary upgrades. A clear understanding of available resources ensures practical solutions are implemented without compromising patient care or operational efficiency.
The goal is to reduce vulnerabilities and improve the facility’s ability to detect, prevent, and respond to incidents. Based on this analysis, a comprehensive proposal outlining new or enhanced security measures can be developed.
Examples of effective healthcare risk mitigation strategies include:
- Observational Practices: Use of surveillance systems and staff policies to monitor high-risk zones and improve real-time threat detection.
- Threat Reporting Tools: Streamlined systems like mobile apps or digital platforms that encourage fast, anonymous, and efficient reporting by staff.
- Security Automations: Implementation of automated systems for alarm triggers, lockdowns, and emergency alerts to ensure immediate action during incidents.
- Continuous Training: Ongoing staff education on safety protocols, threat recognition, and emergency response for improved preparedness and awareness.
Step 4 - Implement New Security Solutions
After finalizing risk mitigation strategies, hospital administrators collaborate with internal security teams and professional integrators to install and configure new security systems. These specialists help combine technologies to provide seamless protection.
Alongside technical improvements, updating or creating organizational policies is vital. These policies must be documented clearly and incorporated into employee training. The assessment findings and related documentation should be stored safely in both digital and physical formats to comply with legal and regulatory standards.
Consider the following questions to guide the implementation across different security domains:
General Security
- What procedures exist for identifying and managing unknown individuals within the hospital?
- Are physical security features like locks, barriers, and signage regularly inspected?
- How do staff members report suspicious behavior or potential threats?
- Are there panic buttons or silent alarms accessible to employees throughout the facility?
- How often are lockdown drills performed, and how quickly can the hospital restrict access in a crisis?
- What visible deterrents, such as signage or lighting, are used to discourage unauthorized activity?
Video Security
- Are surveillance cameras positioned to cover entrances, exits, and vulnerable spots?
- Who is responsible for monitoring video feeds, and during which hours?
- Can authorized staff access live footage remotely when needed?
- How long is video data stored, and how is it protected from tampering?
- Are analytic tools used to detect unusual behavior or patterns in real-time?
- What is the maintenance schedule for cameras and related software?
Access Control
- How are access permissions managed for different departments or restricted zones?
- Does the hospital have a process to verify and track visitors entering sensitive areas?
- Are temporary credentials issued securely and monitored?
- Can the system alert security staff immediately when unauthorized access is attempted?
- Is emergency access granted to first responders without compromising security?
- How are lost or stolen access credentials handled and deactivated?
Security Personnel
- What qualifications and certifications do security staff hold?
- How frequently are security personnel trained on new threats and protocols?
- Are patrol routes planned to cover all critical hospital areas without gaps?
- Is there a communication system that allows guards to quickly report incidents or call for backup?
- How are security incidents recorded, reviewed, and acted upon?
- Do security staff participate in drills simulating emergency situations?
By addressing these questions, hospitals can put into place tailored security solutions that protect patients, staff, and assets from a wide range of threats.
Step 5 - Engage Key Stakeholders Early
During the planning phase, involve department heads, IT teams, clinical staff, HR, and even patient representatives. Their input helps identify on-ground realities and practical challenges. Engaging stakeholders early improves buy-in, promotes smoother implementation, and helps uncover security blind spots often missed by external assessors.
Step 6 - Conduct a Walkthrough and On-Site Inspection
Before drafting recommendations, do a physical and operational walkthrough of the entire hospital. Look at access points, security camera placements, lighting, signage, and staff awareness. This allows assessors to compare policies on paper versus real-world practices and spot unsafe areas or behaviors that may not appear in reports.
Step 7 - Review Incident Response and Communication Protocols
Evaluate how the hospital currently handles emergencies, whether it’s a physical breach, fire, violent patient, or data leak. Assess the clarity and speed of communication between departments, security teams, and law enforcement. This review can highlight delays, confusion, or gaps in command structure during high-pressure situations.
Conclusion
The safety of patients, staff, and hospital property remains a top priority for healthcare organizations. Hospitals must protect against physical and digital threats while meeting strict laws and industry regulations.
A thorough hospital security risk assessment covers many important areas to address all potential risks, including:
- Physical Security Evaluation,
- Risk Assessment & Threat Identification,
- Regulatory Compliance,
- Vulnerability Testing,
- Emergency Preparedness Evaluation
- Technology Integration,
- Policies and Procedures, and
- Staff Training
Regularly reviewing and updating security systems and policies helps hospitals prepare for new challenges. Conducting these assessments gives hospital leaders a clear understanding of existing weaknesses and helps them focus resources on the most urgent security needs.
By following this approach, healthcare facilities can more effectively protect their people and assets and maintain a safer environment for everyone.





%20(1).png)







.webp)
