Think hospitals are just about patient care? They’re also housing sensitive data, expensive equipment, and controlled substances, all while staying open to the public 24/7. That’s a big security puzzle. And when one weak access point can lead to serious risk, basic locks or outdated systems just won’t cut it.
This article will help you understand how modern access control systems strengthen hospital security without slowing down care.
- Different types of access control systems and how they work
- How they protect patients, staff, and sensitive data
- Why Coram is the smarter choice for securing hospitals today
What is Access Control in Hospitals?
Access control in hospitals refers to the systems used to manage who can access specific areas, equipment, or digital records. It ensures that only authorized personnel like doctors, nurses, or IT staff can enter sensitive zones or view confidential data.
There are two main layers of access control:
- Physical access control: Secures spaces like patient wards, pharmacies, and operating rooms using tools like key cards, biometric scanners, or mobile credentials.
- Digital (logical) access control: Controls who can log into systems like electronic health records (EHR), admin portals, or internal databases.
- Identity and Access Management (IAM): A unified approach that applies policies based on job role, time of day, and security clearance across both physical and digital systems.
What Are the Types of Access Control?
Hospitals use different types of access control systems to protect their spaces, staff, and sensitive data. Each type serves a specific function, from keeping intruders out at the gate to controlling who enters restricted medical zones.
The types of access control include:
1. Perimeter Access Solutions
Perimeter access controls manage who can enter the hospital grounds or parking areas.
These include fences, automatic gates, guard-monitored entrances, and badge-controlled parking lots. In larger facilities, license plate recognition and surveillance cameras are used to track vehicles and manage deliveries.
These solutions help prevent unauthorized individuals from casually walking in or gaining vehicle access, especially important for emergency room entrances, ambulance bays, and staff-only zones.
2. Electronic Access Control Systems
Electronic access systems control entry to internal spaces like operating rooms, medicine storage, staff lounges, or data centers.
They rely on devices such as card readers, biometric scanners (like fingerprint or facial recognition), keypad locks, or smartphone-based credentials. Access can be limited by role, shift timings, or location.
These systems automatically record every entry and exit, which helps with audits, investigations, and compliance checks.
3. On-premise Access Control Systems
On-premise systems are managed within the hospital’s own servers and network infrastructure. They don’t rely on the cloud, which gives IT teams full control over data, updates, and configurations.
These are typically used in hospitals with strict internal policies or where internet connectivity isn’t reliable. While they offer greater security and privacy, they require regular maintenance and are harder to scale than cloud-based systems.
4. Lockdown and Emergency Response Systems
These systems are designed to respond quickly during emergencies such as active threats, fires, or biohazard incidents.
Hospitals can trigger partial or full lockdowns, locking doors automatically to contain the situation. Some systems are linked to AI-powered sensors that detect aggression, gunshots, or unauthorized access attempts and initiate lockdowns without human intervention.
These systems help protect staff and patients until help arrives.
5. Hospital Access Control Policies
Policies define how access systems are used and who is allowed where.
They include role-based access levels, visitor management rules, vendor access protocols, and procedures for revoking access when staff leave or change roles. Good policies also define how to handle “break-glass” scenarios where emergency access is required.
These rules ensure that access decisions are consistent and aligned with compliance standards like HIPAA.
Why is Access Control Important in Healthcare?
Access control is critical in healthcare because it protects what hospitals value most: patients, data, and trust. Without the right safeguards, even a small oversight like a misplaced access badge or an unlocked medication room can lead to serious consequences, from safety risks to regulatory violations.
Here’s why access control is crucial in healthcare:
1. Protects Patient Privacy and PHI
Hospitals manage thousands of personal records daily. Access control ensures that only authorized staff can view or edit sensitive patient health information (PHI). This isn’t just about HIPAA; it’s about trust. Patients expect confidentiality from the moment they walk in.
- Only clinicians can access treatment records
- Restricted systems prevent admin staff from seeing medical notes
- Audit trails help detect and report any unauthorized access
2. Secures High-Risk Areas
Not every room should be open to everyone. From operating theaters and ICUs to drug cabinets and server rooms, access must be tightly controlled.
- Medication theft or mishandling is a real risk without proper controls
- Data rooms and diagnostics labs often house sensitive infrastructure
- Emergency protocols rely on locking or isolating zones quickly
3. Keeps Visitors and Vendors in Check
Hospitals are busy, public-facing environments. Without smart access policies, it’s hard to track who’s where and why.
- Visitor badges can expire after specific time slots
- Vendors can be restricted to certain areas only
- Staff can verify identity before granting physical or digital access
4. Boosts Workflow and Efficiency
With automated access control, staff don’t waste time finding keys or waiting for manual clearance.
- Swipe cards or biometrics speed up movement across departments
- Systems can adjust access rights automatically during shift changes
- Integration with HR or scheduling software reduces manual errors
5. Lowers Legal and Compliance Risk
Every unauthorized access event is a potential compliance violation. A missed audit trail or unmonitored system can lead to lawsuits, penalties, or reputation loss.
Robust access control reduces this risk by design.
- Logs prove who accessed what, when, and why
- Helps demonstrate due diligence during audits or breach investigations
- Reduces liability from insider threats or accidental exposure
How Does Access Control in Hospitals Work?
Access control in hospitals works by verifying who someone is, checking what they’re allowed to do, and then either granting or denying access, whether that’s a physical door, a digital record, or a secured zone.
Here’s a step-by-step look at how it functions in a typical hospital setting:
User Identity is verified
Every person, whether staff, vendor, or visitor, is assigned a unique ID. This could be tied to a badge, PIN, biometric scan, or mobile credential. When they try to access a restricted area or system, the control point (a door reader, software login, etc.) checks if the identity is valid.
Permissions are Checked in Real-Time
The system compares the person’s credentials against a pre-defined set of rules usually based on their role, location, time of day, or department.
For example:
- A nurse can enter the ICU but not the pharmacy.
- A lab technician can’t access patient billing data.
- A vendor can only access delivery zones during business hours.
Access is Granted (or Denied)
If the user’s permissions match the requirements, access is granted, usually through an automated door unlock, system login, or device activation. If not, access is denied, and the attempt is logged.
Everything is Tracked and Audited
Every interaction, whether successful or blocked, is recorded. These logs help with audits, investigations, and compliance reporting. Security teams can track patterns, spot unusual behavior, and quickly respond if something feels off.
Systems Are Integrated and Adaptive
In modern hospitals, access control systems often integrate with video surveillance, HR software, or even patient monitoring tools. This helps create a centralized, automated view of security operations, making it easier to scale, respond, and update policies as needed.
In short, access control works quietly in the background, verifying identities, enforcing permissions, and keeping people and data safe without disrupting daily hospital workflows.
Why Coram is the Best Access Control System for Hospitals?
Coram is a purpose-built access control platform designed specifically for hospitals where life moves fast, security risks are high, and downtime isn’t an option. It goes beyond locking doors. Coram ensures the right people have access at the right time, without compromising safety, compliance, or care delivery.
Here’s how each feature solves real problems hospitals face every day:
Real-Time Credentialing
Without live credential updates, hospital staff often face delays at access points, especially during shift changes, department transfers, or emergency situations. Outdated permissions can prevent critical personnel from entering the spaces they need to do their job.
Coram solves this by instantly updating access rights across departments, shifts, and roles. Whether it’s a nurse heading to another floor or a specialist called in during off-hours, they’ll have access when and where it’s needed without waiting on manual approvals.
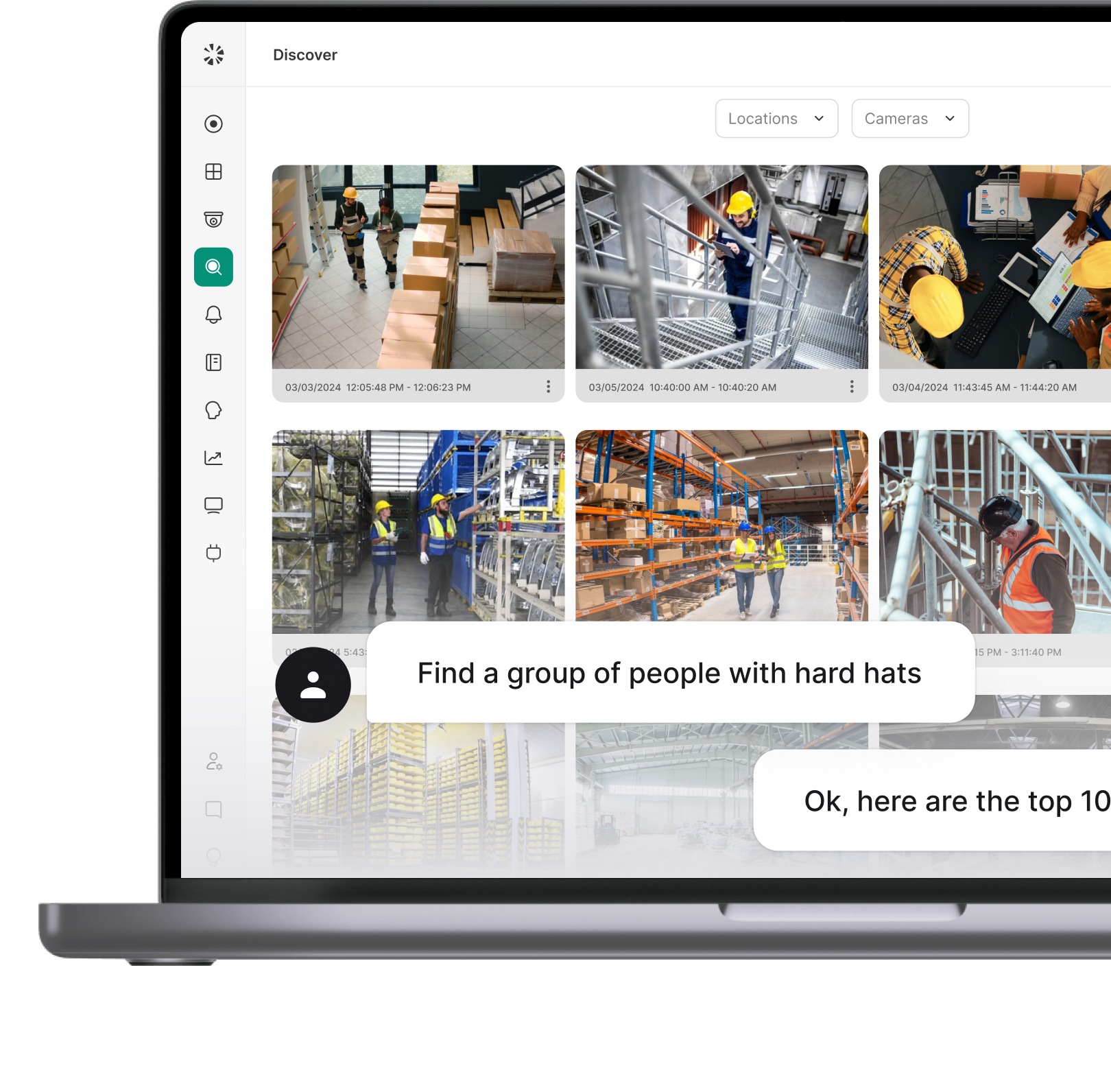
AI-Powered Monitoring and Alerts
Traditional access systems record events but rarely flag issues in real time. That means tailgating, badge misuse, or after-hours entry often goes unnoticed until it's too late.
Coram combines access logs with real-time video surveillance and AI-driven alerts. If a door is forced, an unauthorized person enters a restricted zone, or someone uses a deactivated badge, Coram immediately notifies security, along with visual confirmation.
Automated Permission Management
Manually managing access for hundreds of staff members, especially in rotating shifts or temporary contracts, is time-consuming and error-prone. Missed revocations and over-permissioning are common.
Coram automates access control by syncing with hospital HR systems and shift schedules. Permissions are automatically granted, updated, or revoked based on roles, employment status, and department, reducing admin work and tightening security.
Biometric and Mobile Access Options
Lost badges and shared PINs weaken hospital security. They’re hard to track and make it difficult to verify who actually accessed a space.
Coram supports secure, individual-based authentication using fingerprints, facial recognition, or mobile credentials. No badge? No problem. Staff can use their phones or biometrics for secure, touchless access that’s tied to their identity.
Seamless Integration with Hospital Systems
Disconnected tools create gaps when access control doesn’t sync with HR platforms, EHR systems, or scheduling software, permissions become outdated, and compliance risks increase.
Coram integrates directly with the systems hospitals already use, so access control stays aligned with real-time staff data. It also simplifies audits by maintaining accurate, traceable logs of every access event across systems.
Coram is a secure solution built for how hospitals actually function. From frontline care to backend compliance, it helps facilities stay fast, safe, and in control.
The Benefits of Hospital Access Control Systems
Access control systems in hospitals create safer environments for patients and staff, reduce operational risks, and help facilities stay compliant without slowing anyone down.
Let’s break down the core benefits:
1. Enhanced Security Across Facilities
Hospitals deal with high foot traffic and sensitive areas like ICUs, pharmacies, and record rooms. Without proper controls, the risk of theft, unauthorized entry, and data breaches rises sharply.
Access control systems restrict entry to only authorized personnel, securing critical zones and protecting against internal and external threats. Many systems also log every access attempt, providing a digital trail for investigations or audits.
2. Protection of Patient Data and Privacy
Electronic Health Records (EHRs) and other patient data must be kept confidential, not just for HIPAA compliance, but for trust and safety.
Access control helps enforce role-based access to digital systems, ensuring only the right users have access to sensitive data. It minimizes the risk of information leaks or unauthorized modifications to patient records.
3. Stronger Compliance and Audit Readiness
Healthcare organizations must comply with HIPAA, GDPR, and other data protection regulations. That means proving who accessed what, and when.
Access control systems generate detailed logs and audit trails that help hospitals meet regulatory standards and provide evidence during audits or breach investigations.
4. Real-Time Monitoring and Alerts
Security teams can’t be everywhere. And manual checks can’t catch every breach.
Modern systems offer real-time dashboards, notifications, and alerts for unusual access attempts, expired credentials, or forced entry events. This enables faster incident response and stronger oversight, without hiring more staff.
5. Better Patient Safety in Restricted Zones
Unauthorized access to NICUs, pediatric wards, psych units, or isolation rooms isn’t just a risk; it can be life-threatening.
Access control prevents such breaches by enforcing strict entry permissions for high-risk areas, ensuring only verified staff and approved visitors get through.
6. Fewer Medical Errors and Supply Misuse
When medication rooms and storage cabinets are left unlocked or accessed by the wrong hands, the chances of dosage errors, theft, or misplacement rise.
Restricting access to medication zones using access control systems helps reduce these risks, keeping supplies safe and staff accountable.
7. Operational Efficiency for Staff and Visitors
Manual sign-ins, key tracking, and badge handoffs can clog workflows—especially in large hospitals with 24/7 activity.
Electronic access systems speed up movement across the facility. Staff get in and out of areas faster, and visitors are guided to the right places using integrated visitor management systems.
8. Accountability and Transparency
Who entered the operating room at 2 AM? Was a contractor given temporary access to the server room? These questions shouldn’t take hours to answer.
Access control systems track user actions, badge scans, and door entries down to the second. That level of transparency reduces finger-pointing and improves accountability across the board.
How to Secure Hospitals Without Slowing Response?
Hospitals can strengthen security without slowing response by designing systems that support, not interrupt, care delivery. It’s not about locking things down, but about unlocking smarter workflows that keep both patients and staff protected.
Smarter Access Without Bottlenecks
Long queues at security desks or locked doors during emergencies can cost lives. Instead of hard stops, hospitals should use:
- Role-based digital credentials that update in real time
- Badge access systems that work with shift schedules
- Mobile access or biometric readers for hands-free entry
These systems ensure that only the right people get through, and fast.
Layered Surveillance That Alerts, Not Just Records
Security cameras alone don’t prevent incidents. But when integrated with access logs and real-time alerts:
- You get instant visibility if someone enters a restricted zone
- Security can step in before something goes wrong
- Every entry is time-stamped and traceable
Pairing cameras with access control makes surveillance actionable, not just passive.
Visitor Management That Doesn’t Disrupt Flow
Visitors need to feel welcome, but hospitals also need control. A good visitor system:
- Issues time-limited digital or printed badges
- Logs entries and exits without manual paperwork
- Sends real-time alerts if someone overstays or strays
No security guard guessing who's who. No interruptions in patient zones.
Emergency Protocols That Prioritize Access
In critical events like lockdowns or code reds, access control shouldn’t get in the way of first responders. Instead:
- Systems should support “break-glass” overrides for emergency entry
- Emergency zones should be pre-configured to open or restrict automatically
- Staff should receive alerts and access rights instantly based on the incident type
Security and speed don’t have to be trade-offs; they can be engineered together.
Train Staff to Spot Risks, Not Just Swipe Badges
Tech alone doesn’t secure a hospital. Staff awareness is equally important. Hospitals should:
- Conduct regular drills for both physical and cyber emergencies
- Train staff to recognize suspicious behavior and phishing attempts
- Empower teams to report issues without fear or delay
Every nurse, doctor, and admin becomes a part of the hospital’s defense layer.
Ready to Make Hospital Security Seamless?
You've seen what modern access control can do, from protecting patient data to enabling faster emergency response. Here’s what you can take away from it:
- Access control isn’t optional; it’s the backbone of hospital safety, compliance, and day-to-day operations.
- Physical and digital systems must work together to protect everything from ICUs to login screens.
- Response time matters: your system should be secure without slowing your staff down.
- Role-based access keeps risk low by giving the right people the right access, every time.
If outdated systems are holding you back, Coram makes access control smarter—without the complexity. From perimeter locks to identity-based digital access, it’s built for how hospitals actually run.
FAQ
Access control systems in hospitals manage who can go where, and when, physically or digitally. These systems include electronic badge readers, biometric scanners, smart locks, surveillance integrations, and visitor registration platforms. The goal is to ensure only authorized personnel can access restricted areas like ICUs, pharmacies, data centers, or patient records.
Modern systems often combine physical security with digital permissions. For example, a nurse might use a badge to enter a medication room and a fingerprint to access the hospital’s EHR. This layered setup helps reduce internal threats, manage high-risk zones, and ensure real-time visibility of all access events.
HIPAA requires healthcare organizations to limit physical access to systems and data while allowing authorized personnel to carry out their duties. This means hospitals must design their environments to prevent unauthorized individuals—whether patients, visitors, or staff from accessing protected health information (PHI).
Under HIPAA’s Security Rule, healthcare facilities must implement policies that include:
- Mechanisms to manage physical access to electronic systems
- Validation procedures for staff and contractors
- Contingency access protocols for emergencies.
These controls don’t just apply to IT rooms; they extend to nurses’ stations, admin areas, and even hallways where PHI could be exposed.
Absolutely. Even small practices handle sensitive data, prescription pads, and medical equipment, all of which need protection. Basic access control tools like keypad locks, role-based software access, and simple badge systems can dramatically reduce the risk of theft, breaches, or mishandling.
In fact, access control can help small practices stay compliant with HIPAA, avoid fines, and improve day-to-day efficiency. Instead of guessing who last opened a drug cabinet or who accessed a patient file, teams have a clear audit trail and better accountability without needing large-scale infrastructure.
Role-Based Access Control (RBAC) assigns permissions based on job function. Instead of managing access per individual, hospitals group users into roles such as nurse, surgeon, admin, pharmacist, and give each role specific access rights.
This helps ensure that a receptionist can’t view patient charts or that only pharmacists can unlock storage cabinets. RBAC makes access easier to manage, quicker to audit, and less prone to human error, especially in fast-paced, high-risk environments like healthcare.





.webp)








.webp)